Obstetrics is the field of study concentrated on pregnancy, childbirth and the postpartum period.
Pregnancy
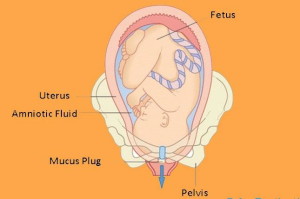
Pregnancy is the term used to describe the period in which a fetus develops inside a woman’s womb or uterus.
Pregnancy usually lasts about 40 weeks, or just over 9 months, as measured from the last menstrual period to delivery. Health care providers refer to three segments of pregnancy, called trimesters. The major events in each trimester are described below.
First Trimester (Week 1 to Week 12)
The events that lead to pregnancy begin with conception, in which a sperm penetrates an egg. The fertilized egg (called a zygote) then travels through the woman’s fallopian tube to the uterus, where it implants itself in the uterine wall. The zygote is made up of a cluster of cells that later form the fetus and the placenta. The placenta connects the mother to the fetus and provides nutrients and oxygen to the fetus.2
Second Trimester (Week 13 to Week 28)
- Between 18 and 20 weeks, the typical timing for ultrasound to look for birth defects, you can often find out the sex of your baby.
- At 20 weeks, a woman may begin to feel movement.
- At 24 weeks, footprints and fingerprints have formed and the fetus sleeps and wakes regularly.
- According to research from the NICHD Neonatal Research Network, the survival rate for babies born at 28 weeks was 92%, although those born at this time will likely still experience serious health complications, including respiratory and neurologic problems.
Third Trimester (Week 29 to Week 40)
- At 32 weeks, the bones are soft and yet almost fully formed, and the eyes can open and close.
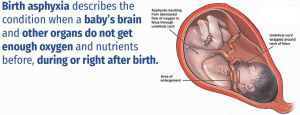
- Infants born before 37 weeks are considered preterm. These children are at increased risk for problems such as developmental delays, vision and hearing problems, and cerebral palsy.Infants born between 34 and 36 weeks of pregnancy are considered to be “late preterm.”
- Infants born in the 37th and 38th weeks of pregnancy—previously considered term—are now considered “early term.” These infants face more health risks than infants who are born at 39 weeks or later, which is now considered full term.
- Infants born at 39 or 40 weeks of pregnancy are considered full term. Full-term infants have better health outcomes than do infants born earlier or, in some cases, later than this period. Therefore, if there is no medical reason to deliver earlier, it is best to deliver at or after 39 weeks to give the infant’s lungs, brain, and liver time to fully develop.
- Infants born at 41 weeks through 41 weeks and 6 days are considered late term.
- Infants who are born at 42 weeks and beyond are considered post term.
Diet in pregnancy:
During pregnancy, the goal is to be eating nutritious foods most of the time,emphasizing the following five food groups: fruits, vegetables, lean protein, whole grains and dairy products.
Fruit and vegetables
Eat plenty of fruit and vegetables because these provide vitamins and minerals, as well as fibre, which helps digestion and prevents constipation.Cook vegetables lightly in a little water, or eat them raw but well washed, to get the benefit of the nutrients they contain.
Protein
Foods containing protein help the baby grow. Sources of protein include beans, legumes/beans, nuts., eggs,meat (but avoid liver) and fish.
Whole grains. These grains are either present in their whole form or ground into a flour while retaining all parts of the seed (bran, germ and endosperm).Examples of whole grains include Barley,Brown rice,Buckwheat,Bulgur (cracked wheat),Millet,Oatmeal and Whole-wheat bread, pasta or crackers.
Dairy
Aim for three to four servings of dairy foods a day. Dairy foods, such as milk, yoghourt and cheese, are good dietary sources of calcium, protein and vitamin D.
Foods to avoid in pregnancy
- When you are pregnant, you should reduce your intake of:
foods that are high in sugar, such as chocolate, biscuits, pastries, ice-cream, cake, puddings and soft drinks. Sugar contains calories without providing any other nutrients, and can contribute to weight gain, obesity and tooth decay - foods that are high in fat, such as all spreading fats (including butter), oils, salad dressings and cream. Fat is very high in calories, and eating more fatty foods is likely to make you put on weight. Having too much saturated fat can increase the amount of cholesterol in the blood, which increases the chance of developing heart disease.
- Foods that contain added salt. Don’t add salt in cooking or at the table.It can contribute to high blood pressure.
Exercise in Pregnancy:
Exercise is not dangerous for your baby. There is some evidence that active women are less likely to experience problems in later pregnancy and labour.The more active and fit you are during pregnancy, the easier it will be for you to adapt to your changing shape and weight gain. It will also help you to cope with labour and get back into shape after the birth.
As a general rule, you should be able to hold a conversation as you exercise when pregnant. If you become breathless as you talk, then you’re probably exercising too strenuously.
Stomach-strengthening exercises
As your baby gets bigger, you may find that the hollow in your lower back increases and this can give you backache. These exercises strengthen stomach (abdominal) muscles and may ease backache, which can be a problem in pregnancy:
- start in a box position (on all 4s) with knees under hips, hands under shoulders, with fingers facing forward and abdominals lifted to keep your back straight
- pull in your stomach muscles and raise your back up towards the ceiling, curling your trunk and allowing your head to relax gently forward. Do not let your elbows lock
- hold for a few seconds then slowly return to the box position
- take care not to hollow your back: it should always return to a straight/neutral position
- do this slowly and rhythmically 10 times, making your muscles work hard and moving your back carefully
- only move your back as far as you can comfortably
Pelvic tilt exercises
- stand with your shoulders and bottom against a wall
- keep your knees soft
- pull your tummy button towards your spine, so that your back flattens
- against the wall: hold for 4 seconds then release
- repeat up to 10 times
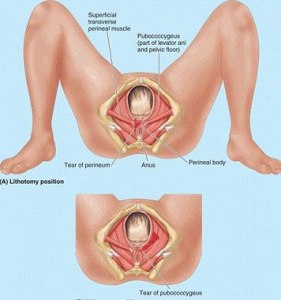
Pelvic floor exercises
- Pelvic floor exercises help to strengthen the muscles of the pelvic floor, which come under great strain in pregnancy and childbirth.).If your pelvic floor muscles are weak, you may find that you leak urine when you cough, sneeze or strain. This is quite common, and there is no reason to feel embarrassed. It’s known as stress incontinence and it can continue after pregnancy.You can strengthen these muscles by doing pelvic floor exercises. This helps to reduce or avoid stress incontinence after pregnancy. All pregnant women should do pelvic floor exercises, even if you’re young and not suffering from stress incontinence now.
How to do pelvic floor exercises:
- close up your bottom, as if you’re trying to stop yourself going to the toilet
- at the same time, draw in your vagina as if you’re gripping a tampon, and your urethra as if to stop the flow of urine
- at first, do this exercise quickly, tightening and releasing the muscles immediately
- then do it slowly, holding the contractions for as long as you can before you relax: try to count to 10
- try to do 3 sets of 8 squeezes every day: to help you remember, you could do a set at each meal.
Complications of pregnancy
- Some common complications of pregnancy include, but are not limited to, the following.
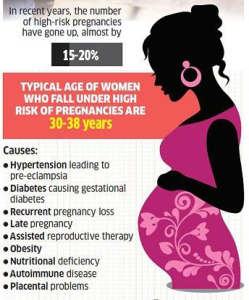
- High Blood Pressure
- Gestational Diabetes
- Infections
- Preeclampsia
- Preterm Labor
- Depression & Anxiety
- Pregnancy Loss/Miscarriage
- Stillbirth
- Other Complications-Severe, persistent nausea and vomiting