The field of gynecology focuses on all other aspects of a woman’s reproductive health from the onset of puberty through menopause and beyond.Gynecologist diagnoses and treats diseases of the reproductive organs including cancer of the ovaries, uterus, cervix, vagina and fallopian tubes. A gynaecologist also treats prolapse of the pelvic organs. This is a condition usually present in postmenopausal women with weakened pelvic muscles that cannot support the uterus or bladder properly.
Common gynaecological problems include:
- Dysmenorrhea/Menstrual Disorders.
- Uterine Fibroids.
- Pelvic Floor Prolapse.
- Pelvic Pain.
- Urinary Incontinence.
- Gynecologic malignancy
Dysmenorrhea/Menstrual Disorders:-
Every woman has a different menstrual cycle. For some, it might occur at the start of every month or the end of every month. Irregular periods, occurs when someone’s menstrual cycle is shorter than 24 days or longer than 38 days or the duration of the cycle varies frequently. Irregular periods are common for teenage girls. They might be irregular periods before they become regular for the first few years. It may also occur in women during perimenopause
- Primary dysmenorrhea. This occurs when you first start your period and continues throughout your life. It is usually life-long. It can cause severe and frequent menstrual cramping from severe and abnormal uterine contractions.
- Secondary dysmenorrhea. This type is due to some physical cause. It usually starts later in life. It may be caused by another medical condition, such as pelvic inflammatory disease,endometriosis,Uterine polyps or fibroids,Stress and lifestyle factors,Birth control pills.
Symptoms:
- Menstrual cycle changes too often
- Period after every 21 days or after every 35 days
- Period lasts more than one week
- Much pain during periods
- Haven’t had a period for 60 days
- Loose more or less blood over a period than usual
- Bleeding in between your periods or following sex
Causes:
- Stress: Multiple studies have shown that a high level of anxiety for a prolonged can lead to irregular periods.
- Obesity: This is also one of the common reasons for irregular periods. The extra fat in the body makes the hormone known as estrogen. The extra dose of estrogen changes the menstrual cycle and can cause irregular periods.
- Hormonal imbalances: Estrogen and progesterone regulate the build-up of the uterus lining. So, if there is a hormonal imbalance in your body, this also results in irregular periods.
- Polycystic ovary syndrome (PCOS): PCOS is one of the reasons for multiple ovarian cysts, hormonal imbalance, and irregular periods.
- Primary ovarian insufficiency (POI): This occurs when ovaries stop working before 40. This may result in irregular periods.
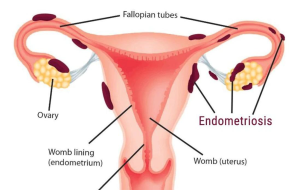
- Endometriosis: This is a condition in which the tissues inside the uterus grows in other parts of the body, causing irregular periods.
- Eating disorders: If you have eating disorders like anorexia or bulimia, you may experience irregular periods.
- Birth control pills: Going on or off birth control pills can cause irregular periods.
Obesity & Polycystic Ovary Syndrome (PCOS):
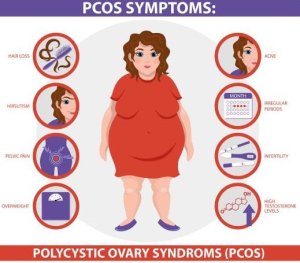
One in every 10 women in India has polycystic ovary syndrome (PCOS), a common endocrine system disorder among women of reproductive age, according to a study by PCOS Society. And out of every 10 women diagnosed with PCOS, six are teenage girls.
Obesity is associated with PCOS and can worsen complications of the disorder.
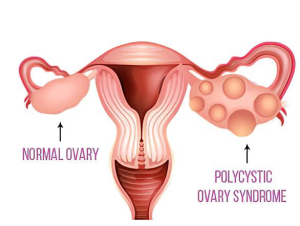
What is PCOS?
Polycystic ovary syndrome or PCOS is a hormonal disbalance in women who are of reproductive age. In this condition, the ovaries of the woman may become enlarged and they may develop numerous harmless fluid filled sacs (follicles). These follicles are underdeveloped sacs which are meant for developing eggs – when you have PCOS, these follicles fail to release the matured eggs.
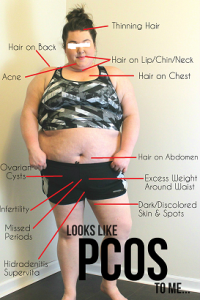
Common symptoms of PCOS
PCOS is very common in recent days and affects many women. While these symptoms can be treated, some women do not even face any of the symptoms, thus it may go undiagnosed. The symptoms of PCOS can get worse if one is overweight or obese. Here are some symptoms of PCOS that you can notice:
- Irregular periods or no periods at all
- Excessive pain during periods accompanied with heavy flow
- Hirsutism i.e. growth of hair on the face, back, chest or butt
- Acne
- Thinning of hair or hair loss resulting in male pattern baldness
- Excessive weight gain
- Difficulty in conceiving
- Pain in the pelvic area
- Anxiety and depression
- High blood sugar and high blood pressure
Complications of PCOS can include:
- Infertility
- Gestational diabetes or pregnancy-induced high blood pressure
- Miscarriage or premature birth
- Nonalcoholic steatohepatitis — a severe liver inflammation caused by fat accumulation in the liver
- Metabolic syndrome — a cluster of conditions including high blood pressure, high blood sugar, and abnormal cholesterol or triglyceride levels that significantly increase your risk of cardiovascular disease
- Type 2 diabetes or prediabetes
- Sleep apnea
- Depression, anxiety and eating disorders
- Abnormal uterine bleeding
- Cancer of the uterine lining (endometrial cancer)
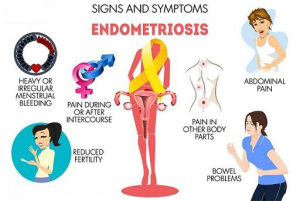
Endometriosis:
Its painful disorder in which tissue similar to the tissue that normally lines the inside of your uterus — the endometrium — grows outside your uterus. Endometriosis most commonly involves ovaries, fallopian tubes and the tissue lining your pelvis.
Symptoms
- Acute pain in lower abdomen or back pain during periods
- Pain in lower abdomen or back pain during non-period days also (this happens in chronic cases)
- Heavy periods,frequent periods or early periods
- Bleeding in between periods (breakthrough bleeding)
- Passing clots during periods
- Painful urination
- Painful defecation
- Painful intercourse
- Mood swings
- Depression
- Infertility
Treatment: Endometriosis has no cure, but its symptoms can be managed.
Medical and surgical options are available to help reduce your symptoms and manage any potential complications.
- Pain medications
- Hormone therapy.
- Hormonal contraceptives
- Gonadotropin-releasing hormone (GnRH) agonists and antagonists
- Danazol.
Conservative surgery
Conservative surgery is typically used for people who want to get pregnant or who experience severe pain and hormonal treatments are not working. The goal of conservative surgery is to remove or destroy endometrial growths without damaging the reproductive organs.
Laparoscopy, a minimally invasive surgery, is used to both visualize and diagnose endometriosis. It is also used to remove the abnormal or displaced endometrial-like tissue. A surgeon makes small incisions in the abdomen to surgically remove the growths or to burn or vaporize them.
Last-resort surgery (hysterectomy)
Your doctor may recommend a total hysterectomy as a last resort if your condition does not improve with other treatments.
During a total hysterectomy, a surgeon removes the uterus and cervix. They also remove the ovaries because these organs make estrogen, and estrogen can cause the growth of endometrial-like tissue. Additionally, the surgeon removes visible implant lesions.
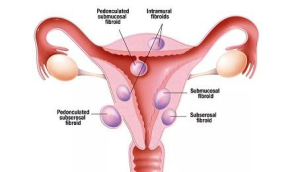
Uterine Fibroids
Uterine fibroids are a common type of noncancerous tumour that can grow in and on your uterus. Not all fibroids cause symptoms, but when they do, symptoms can include heavy menstrual bleeding, back pain, frequent urination and pain during sex. Small fibroids often don’t need treatment, but larger fibroids can be treated with medications
or surgery.
Risk factors:
- Obesity and a higher body weight (a person is considered obese if they’re more than 20% over the healthy body weight).
- Family history of fibroids.
- Not having children.
- Early onset of menstruation (getting your period at a young age).
- Late age for menopause.
Signs & symptoms:
- Excessive or painful bleeding during your period (menstruation).
- Bleeding between your periods.
- A feeling of fullness in your lower abdomen/bloating.
- Frequent urination (this can happen when a fibroid puts pressure on your bladder).
- Pain during sex.
- Low back pain.
- Constipation.
- Chronic vaginal discharge.
- Inability to urinate or completely empty your bladder.
- Increased abdominal distention (enlargement), causing your abdomen to look pregnant.
Treatment: Treatment plan will depend on a few factors, including:
- How many fibroids you have.
- The size of your fibroids.
- Where your fibroids are located.
- What symptoms you are experiencing related to the fibroids.
- Your desire for pregnancy.
- Your desire for uterine preservation.
Medications
- Medications for pain: These medications can be used to manage discomforts and pain caused by the fibroids.
- Iron supplements: If you have anemia from the excess bleeding, your provider may also suggest you take an iron supplement.
- Birth control: Birth control can also be used to help with symptoms of fibroids — specifically heavy bleeding during and between periods and menstrual cramps. Birth control can be used to help control heavy menstrual bleeding. There are a variety of birth control options you can use, including oral contraceptive pills, intravaginal contraception, injections and intrauterine devices (IUDs).
- Gonadotropin-releasing hormone (GnRH) agonists: These medications can be taken via a nasal spray or injection and they work by shrinking your fibroids. They’re sometimes used to shrink a fibroid before surgery, making it easier to remove the fibroid. However, these medications are temporary and if you stop taking them, the fibroids can grow back.
- Oral therapies: Elagolix is a new oral therapy indicated for the management of heavy uterine bleeding in premenopausal women with symptomatic uterine fibroids. It can be used up to 24 months. Talk to your doctor for pros and cons of this therapy. Another oral therapy, Tranexamic acid, is an antifibrinolytic oral drug that’s indicated for the treatment of cyclic heavy menstrual bleeding in women with uterine fibroids. Your doctor will monitor you during this therapy.
It’s important to talk to Doctor about any medication you take.
Always consult your Doctor before starting a new medication to discuss any possible complications.
Fibroid surgery
There are several factors to consider when talking about the different types of surgery for fibroid removal. Not only can the size, location and number of fibroids influence the type of surgery, but your wishes for future pregnancies can also be an important factor when developing a treatment plan. Some surgical options preserve the uterus and allow you to become pregnant in the future, while other options can either damage or remove the uterus.
Myomectomy is a procedure that allows your provider to remove the fibroids without damaging the uterus. There are several types of myomectomy. The type of procedure that may work best for you will depend on where your fibroids are located, how big they are and the number of fibroids. The types of myomectomy procedure to remove fibroids can include:
Menopause:
Menopause is the time that marks the end of your menstrual cycles. It’s diagnosed after you’ve gone 12 months without a menstrual period.Menopause is a natural biological process. But the physical symptoms, such as hot flashes, and emotional symptoms of menopause may disrupt your sleep, lower your energy or affect emotional health. There are many effective treatments available, from lifestyle adjustments to hormone therapy.
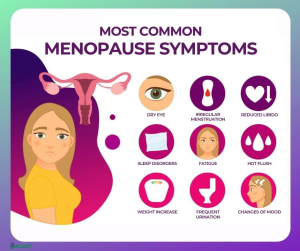
Symptoms
In the months or years leading up to menopause (perimenopause), you might experience these signs and symptoms:
- Irregular periods
- Vaginal dryness
- Hot flashes
- Chills
- Night sweats
- Sleep problems
- Mood changes
- Weight gain and slowed metabolism
- Thinning hair and dry skin
- Loss of breast fullness
Signs and symptoms, including changes in menstruation can vary among women. Most likely, you’ll experience some irregularity in your periods before they end.
Skipping periods during perimenopause is common and expected. Often, menstrual periods will skip a month and return, or skip several months and then start monthly cycles again for a few months. Periods also tend to happen on shorter cycles, so they are closer together. Despite irregular periods, pregnancy is possible. If you’ve skipped a period but aren’t sure you’ve started the menopausal transition, consider a pregnancy test.
When to see a doctor
Keep up with regular visits with your doctor for preventive health care and any medical concerns. Continue getting these appointments during and after menopause.
Preventive health care as you age may include recommended health screening tests, such as colonoscopy, mammography and triglyceride screening. Your doctor might recommend other tests and exams, too, including thyroid testing if suggested by your history, and breast and pelvic exams.
Always seek medical advice if you have bleeding from your vagina after menopause.
Complications
After menopause, your risk of certain medical conditions increases. Examples include:
- Heart and blood vessel (cardiovascular) disease. When your oestrogen levels decline, your risk of cardiovascular disease increases. Heart disease is the leading cause of death in women as well as in men. So it’s important to get regular exercise, eat a healthy diet and maintain a normal weight. Ask your doctor for advice on how to protect your heart, such as how to reduce your cholesterol or blood pressure if it’s too high.
- Osteoporosis. This condition causes bones to become brittle and weak, leading to an increased risk of fractures. During the first few years after menopause, you may lose bone density at a rapid rate, increasing your risk of osteoporosis. Postmenopausal women with osteoporosis are especially susceptible to fractures of their spine, hips and wrists.
- Urinary incontinence. As the tissues of your vagina and urethra lose elasticity, you may experience frequent, sudden, strong urges to urinate, followed by an involuntary loss of urine (urge incontinence), or the loss of urine with coughing, laughing or lifting (stress incontinence). You may have urinary tract infections more often.
Strengthening pelvic floor muscles with Kegel exercises and using a topical vaginal estrogen may help relieve symptoms of incontinence. Hormone therapy may also be an effective treatment option for menopausal urinary tract and vaginal changes that can result in urinary incontinence. - Sexual function. Vaginal dryness from decreased moisture production and loss of elasticity can cause discomfort and slight bleeding during sexual intercourse. Also, decreased sensation may reduce your desire for sexual activity (libido).
Water-based vaginal moisturizers and lubricants may help. If a vaginal lubricant isn’t enough, many women benefit from the use of local vaginal estrogen treatment, available as a vaginal cream, tablet or ring. - Weight gain. Many women gain weight during the menopausal transition and after menopause because metabolism slows. You may need to eat less and exercise more, just to maintain your current weight.
Nutrition after menopause
Dairy Products- The decline in estrogen levels during menopause can increase women’s risk of fractures.Dairy products, such as milk, yogurt and cheese, contain calcium, phosphorus, potassium, magnesium and vitamins D and K — all of which are essential for bone health.
Low Fats
- fat free cheese.
- fat free or “skim” milk or yogurt.
- light or fat free cream cheese.
- low fat cottage cheese, milk, or yogurt.
- Omega-3 fatty acids, may benefit women going through menopause
Whole Grains
Whole grains are high in nutrients, including fiber and B vitamins, such as thiamine, niacin, riboflavin and pantothenic acid A diet high in whole grains has been linked to a reduced risk of heart disease, cancer and premature death.
Fruits and Vegetables
Fruits and vegetables are packed with vitamins and minerals, fiber and antioxidants.
Phytoestrogen-Containing Foods
Phytoestrogens are compounds in foods that act as weak estrogens in your body.
Foods that naturally contain phytoestrogens include soybeans, chickpeas, peanuts, flax seeds, barley, grapes, berries, plums, green and black tea.
Protein
The decline in estrogen from menopause is linked to decreased muscle mass and bone strength.Foods high in protein include all types of beans, eggs, meat, fish and dairy products
Share on Pi
Pelvic inflammatory disease (PID):
- It is infection of reproductive organs like uterus, ovaries and fallopian tubes.

Causes:
- The main cause of PID is through a sexually transmitted infection (STI) such as chlamydia, gonorrhoea or mycoplasma genitalium.
- Following childbirth or a miscarriage
- Diabetes
- After insertion of an intrauterine device (IUD)
- Have more than 1 sexual partner
- Have a new sexual partner
Symptoms:
- Pain in your lower belly and pelvis
- Nausea, Vomiting
- Fever and chills
- Heavy discharge from your vagina(whitish ,brownish) with an unpleasant odour
- More bleeding than usual during your period
- Bleeding between periods
- Pain during sex
- Pain while micturition or passing stools

Complications:
- Ectopic pregnancy. PID is a major cause of tubal (ectopic) pregnancy
- Infertility. Damage to your reproductive organs may cause infertility — the inability to become pregnant.
- Chronic pelvic pain. Pelvic inflammatory disease can cause pelvic pain that might last for months or years.
- Tubo-ovarian abscess.
Gynecologic malignancy:
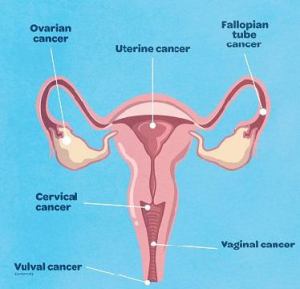
1. Uterine cancer:
Uterine cancer is cancer that begins in the uterus and is one of the most common types of gynecological cancers. Though it can happen to anyone, some factors which increase the risk of uterine cancer are obesity, diabetes, hypertension, use of estrogen without progesterone, etc.
THE COMMON ENDOMETRIAL CANCER SYMPTOMS ARE:
- Vaginal bleeding or spotting after menopause.
- Pain in the lower abdomen that persists for more than two weeks.
- Bleeding between periods.
- Pain during sexual intercourse.
Uterine cancers can be further subdivided into endometrial cancers, uterine sarcomas, and endometrial stromal tumours. Of these, endometrial cancer is the most common type of uterine cancer and the other two are quite rare. Endometrial cancer is also one of the most curable ones.
Endometrial cancer is diagnosed quite early in most cases and hence is treated by a laparoscopic (minimally invasive) surgery. The entire treatment requires only 2-3 days of hospital stay in most cases. Though a few patients of endometrial cancer (about 10-15%) may require further treatment in the form of radiotherapy or a combination of radiotherapy and chemotherapy.
2. Cervical cancer:
Another very common type of gynecologic cancer is cervical cancer and is one of the leading causes of cancer-related deaths in women worldwide. A large number of women in India are diagnosed with this cancer every year, and unfortunately, due to lack of awareness and poor cancer screening facilities, a majority of women are diagnosed when cancer has reached advanced stages. Also, a large number of cervical cancers are caused due to HPV (Human Papillomavirus) infection.
SOME COMMON CERVICAL CANCER SYMPTOMS INCLUDE:
- Vaginal discharge.
- Vaginal odour.
- Bleeding after sexual intercourse.
- Abnormal vaginal bleeding.
Regular cancer screenings and PAP test for HPV detection are important for early detection. If diagnosed early, cervical cancer can be treated by radical surgery alone while those detected in advanced stages require a combination of chemo and radiation therapy.
Vaccinating young girls for preventing HPV infection before they are sexually active is a very effective way to prevent cervical cancers as well as many other forms of gynecological cancers.
3. Ovarian cancer:
Ovarian cancer is another common gynecological cancer. There are three types of it: epithelial ovarian cancer, germ cell cancer, and stromal cell cancer. Of these, epithelial ovarian cancer is the most common one accounting for about 85 percent of all ovarian cancers.
SOME COMMON OVARIAN CANCER SYMPTOMS ARE:
- Extreme and sudden onset of bloating.
- Difficulty in eating or loss of appetite.
- Unexplained weight loss
- Increased frequency or urgency of urination.
- Pain and discomfort in the pelvic or abdominal region.
The benign epithelial ovarian tumours can be cured by surgery and the malignant ones are treated by tumour cytoreductive surgery and chemotherapy. One important point to note about epithelial ovarian cancers is that they are quite aggressive and have a tendency to recur in an advanced stage. In such cases, treatment is done either surgically or through chemotherapy.
Germ cell tumour, another type of ovarian cancer, is usually seen in younger individuals and about 95% of these are curable by surgery alone while other cases may require additional chemotherapy. To treat germ cell tumour in young patients, fertility preservation therapy (sparing the other ovary and uterus) is usually preferred for treatment.
The third type of ovarian cancer i.e. the stromal cell cancer is usually slow-growing in nature. A majority of such cases are treatable by surgery alone.
RARE GYNECOLOGICAL CANCERS:
Some rarer forms of gynecological cancers are:
1. Vulvar cancer:
Vulvar cancer is a rare form of gynecological cancer and it affects the external female genitalia. It usually occurs in elderly women and is easily identifiable by the following symptoms:
- Red, pink, or white bumps having wart-like surface.
- Pain or burning sensation while urinating.
- Bleeding not associated with menstruation.
- Presence of white and rough patch in the region.
- A persistent open sore or ulcer.
Vulvar cancer is a highly curable type of gynecological cancer. In most cases, radical surgery is sufficient to treat vulvar cancer but some cases may require chemotherapy and radiation therapy as well.
2. Vaginal cancer:
Vaginal cancer is one of the rarest forms of gynecological cancer. It usually affects women over 50 years of age and in most cases, HPV (Human Papillomavirus) infection is responsible for cancer. The symptoms are:
- Presence of an obvious mass.
- Abnormal vaginal bleeding or discharge.
- Pain during and after intercourse.
Similar to vulvar cancer, many cases of vaginal cancers are treatable with radical surgery while others may require radiotherapy and chemotherapy.
3. Gestational trophoblastic tumour:
Gestational trophoblastic disease (GTD) is a term used for a group of pregnancy-related tumours. These type of tumours are also quite rare and are further subdivided into five types (one benign and four malignant). These tumours usually start in the cells that would become placenta during pregnancy. The tumour starts in layers of cells known as trophoblast which surround the embryo and is mostly benign. These tumours are highly curable and are mostly treated with chemotherapy.
When it comes to the diagnosis and gynecological cancers treatment, Cytecare provides you with unparalleled services. At Cytecare, we have a dedicated unit for women’s oncology and our diverse team includes gynecologists, oncologists, radiation oncologists, etc. who have years of experience in treating various gynecological cancers. Our medical expertise is complemented by state-of-the-art infrastructure providing you with the most advanced diagnostic facilities.
COSMETIC GYNECOLOGY / MOMMY MAKEOVER
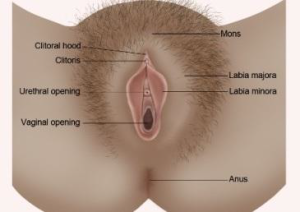
External anatomy of the female genitalia
Vaginal laxity/ Loose vagina:-
Multiple Pregnancies and vaginal delivery can lead to trauma and stretching, which can result in loss of vaginal tightness.
Symptoms
Symptoms include loss of sensation with intercourse and decreased sexual satisfaction. Vaginal laxity can lead to a negative impact on female sexual function, body image and quality of life. The condition is poorly recognized and frequently under-reported.
