Tests for men
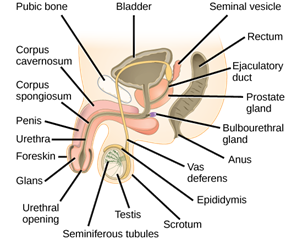
Male fertility requires that the testicles produce enough healthy sperm, and that the sperm is ejaculated effectively into the vagina and travels to the egg. Tests for male infertility attempt to determine whether any of these processes are impaired.
You may have a general physical exam, including examination of your genitals. Specific fertility tests may include:
- Semen analysis. Your doctor may ask for one or more semen specimens. Semen is generally obtained by masturbating or by interrupting intercourse and ejaculating your semen into a clean container. A lab analyzes your semen specimen. In some cases, urine may be tested for the presence of sperm.
- Hormone testing. You may have a blood test to determine your level of testosterone and other male hormones.
- Genetic testing. Genetic testing may be done to determine whether there’s a genetic defect causing infertility.
- Testicular biopsy. In select cases, a testicular biopsy may be performed to identify abnormalities contributing to infertility or to retrieve sperm for assisted reproductive techniques, such as IVF.
- Imaging. In certain situations, imaging studies such as a brain MRI, transrectal or scrotal ultrasound, or a test of the vas deferens (vasography) may be performed.
- Other specialty testing. In rare cases, other tests to evaluate the quality of the sperm may be performed, such as evaluating a semen specimen for DNA abnormalities.
Tests for women
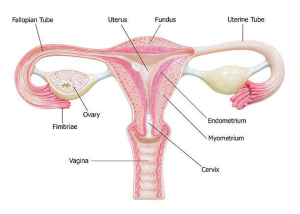
Fertility for women relies on the ovaries releasing healthy eggs. The reproductive tract must allow an egg to pass into the fallopian tubes and join with sperm for fertilization. The fertilized egg must travel to the uterus and implant in the lining. Tests for female infertility try to find out if any of these processes are impaired.
You may have a general physical exam, including a regular gynecological exam. Specific fertility tests may include:
- Ovulation testing. A blood test measures hormone levels to determine whether you’re ovulating.
- Hysterosalpingography. Hysterosalpingography (his-tur-o-sal-ping-GOG-ruh-fee) evaluates the condition of your uterus and fallopian tubes and looks for blockages or other problems. X-ray contrast is injected into your uterus, and an X-ray is taken to determine if the cavity is normal and to see if the fluid spills out of your fallopian tubes.
- Ovarian reserve testing. This testing helps determine the quantity of the eggs available for ovulation. This approach often begins with hormone testing early in the menstrual cycle.
- Other hormone testing. Other hormone tests check levels of ovulatory hormones, as well as pituitary hormones that control reproductive processes.
- Imaging tests. Pelvic ultrasound looks for uterine or ovarian disease. Sometimes a sonohysterogram, also called a saline infusion sonogram, is used to see details inside the uterus that are not seen on a regular ultrasound.
Depending on your situation, rarely your testing may include:
- Hysteroscopy. Depending on your symptoms, your doctor may request a hysteroscopy to look for uterine disease. During the procedure, your doctor inserts a thin, lighted device through your cervix into your uterus to view any potential abnormalities.
- Laparoscopy. This minimally invasive surgery involves making a small incision beneath your navel and inserting a thin viewing device to examine your fallopian tubes, ovaries and uterus. A laparoscopy may identify endometriosis, scarring, blockages or irregularities of the fallopian tubes, and problems with the ovaries and uterus.
Not everyone needs to have all, or even many, of these tests before the cause of infertility is found. You and your doctor will decide which tests you will have and when.